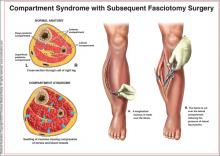
Acute compartment syndrome (ACS) is a condition in which elevated pressures in the confined space of a closed fascial compartment lead to vascular compromise. Typically, ACS develops in the distal extremities after a traumatic event, such as a fracture, crush, or burn injury. A dangerous cycle ensues, involving increased compartmental pressure, decreased tissue perfusion, and continuing ischemia; fluids leak from the vasculature, perpetuating the process.1
Diagnosis of ACS requires a high level of clinical suspicion combined with a keen understanding of the risk factors for ACS and its pathophysiology, as well as astute awareness of the subtle clinical exam findings that usually accompany objective pressure measurements. Though most common in the extremities, ACS may also develop in the buttock, pelvis, or abdominal or spinal musculature.2-5
Prompt recognition and management of ACS are critical: This condition is considered a surgical emergency requiring immediate attention. Urgent decompression by fasciotomy is the definitive treatment6—an essential intervention to prevent critical tissue ischemia and necrosis. Failure to release the fascia in a timely manner can result in poor outcomes for patients, including but not limited to chronic pain, paralysis, sensory or motor deficits, loss of limb, deformity, and renal failure secondary to rhabdomyolysis.7,8
Clinical assessment and severity of injury are the two main factors that lead to prompt diagnosis and treatment of ACS. However, distracting injuries or an unconsciousness patient may interfere with the assessment, decreasing its accuracy.7 Heightened awareness of ACS is paramount so that clinicians can better recognize the condition before complications arise.
EPIDEMIOLOGY
ACS is typically associated with long bone injuries after significant trauma or crush injuries (eg, in a motor vehicle collision). Less often, severe burns, gun shot wounds, snake bites, poor anticoagulation, prolonged surgery (including procedures involving prolonged elevation of a limb),9 nephrotic syndrome, IV infiltrations, and other volume-expanding pathologies can present a similar risk.10-15 Essentially, ACS is a self-perpetuating process resulting from either increased compartmental content (eg, bleeding, edema) or reduced compartment size (eg, tight casting, burns).7,16
Ninety percent of cases of ACS in the extremities occur in men,15 and males younger than 35 have the greatest incidence of posttraumatic ACS.15,17,18 Although fractures account for nearly 70% of confirmed cases of ACS, soft-tissue injuries (particularly vascular injuries15) are also associated with ACS.18 Clinicians should be aware of a key misconception: that open fractures relieve intracompartmental pressure, reducing the risk for ACS. Rather, the damage and inflammation that occur in open fractures pose the same risk for ACS as do closed fractures.15
PATIENT PRESENTATION
A key consideration, in addition to the history and mechanism of injury or illness, is that patient’s description of the pain: The conscious patient will complain of pain that worsens progressively over time and that usually seems out of proportion to the physical exam findings or apparent injury.19 For this reason, serial assessments are recommended; worsening pain is indicative of rapid evolution of ACS, with the possibility of irreversible necrosis.20
Pain with passive stretch is an excellent indicator that the pathology is progressing.2 The “classic P” signs and symptoms of ACS are progressively later findings that represent markedly significant ischemia and injury already in progress: paresthesia, paresis/paralysis, poikilothermia (the inability of the patient to maintain a constant core temperature), pulselessness, and pallor.17
Diminishment of pain suggests a poor prognosis, as this indicates that the tissue is likely nonviable and necrotic by that point.1
Clinicians must be mindful that, in patients with central or peripheral nerve deficits or in those who have undergone nerve blocks or regional anesthesia, pain may be absent; in these instances, the risk for delayed diagnosis is increased.14,21 Furthermore, pain tolerance varies among patients, and distracting injuries may also cloud the clinical picture.
The diagnosis of ACS is not easily made. Thus, clinical suspicion should be elevated in any high-energy scenario: an extensive burn, overly restrictive casting, or volume-expanding disorder—especially in patients who present with pain that is out of proportion to the injury or is worsening progressively.1,7
PHYSICAL EXAMINATION
Physical examination and assessment should be repeated every two to four hours. The examining clinician should focus on pain characteristics, the skin, and the “classic P” signs mentioned above. Marked tenderness out of proportion to the injury, unmanageable pain, and pain on passive movement of the limb are the strongest indicators of developing ACS. These findings are nearly universal in the conscious patient, but they can be confused with primary pain of the injury itself. Additional findings of sensory or motor impairments may help raise the clinician’s suspicion for ACS but are nonspecific.1,7,23 Palpable tenseness is a common observation in ACS, but a clinician’s subjective measurement of skin firmness has little value as an objective strategy.22 Absence of distal pulses, decreased skin temperature, and pallor are very late signs that pressures are sufficiently high to cause complete arterial occlusion.20 Thus, clinicians should not wait for absent pulses or pallor to begin treatment. Suspicion for ACS should arise as soon as pain associated with trauma or surgery intensifies or becomes unmanageable.